Expanding SGLT2 inhibitor use in CKD: Why and how?

Early detection of chronic kidney disease (CKD) enables early optimization of organ-protective treatment to help avert the substantial healthcare burden associated with the condition. At an industry-sponsored symposium organized by the Asian Pacific Society of Nephrology (APSN), Professor See-Cheng Yeo of Tan Tock Seng Hospital, Singapore, and Professor Meg Jardine of the University of Sydney, Australia, discussed evidence supporting earlier and broader use of sodium-glucose cotransporter 2 (SGLT2) inhibitors (eg, empagliflozin) in CKD, highlighting guideline recommendations for SGLT2 inhibitors as first-line (1L) therapy in diabetic kidney disease (DKD) patients with estimated glomerular filtration rate (eGFR) ≥20 mL/min/1.73 m2.
Stage 3 CKD underdiagnosed
Despite the increasing incidence and prevalence of CKD worldwide, large proportions
of patients with stage 3 disease remain undiagnosed (Japan, 92.1 percent;
US, 61.6–64.3 percent; Italy, 77.0 percent; Germany, 84.3 percent; France,
95.5 percent). [Lancet 2020;395:709- 733;
BMJ Open 2023;13:e067386]
“There are substantial opportunities to improve diagnosis of stage 3 CKD. The low diagnosis rates in patients with comorbidities put them at increased risks of CKD progression and complications,” said Yeo. [BMJ Open 2023;13:e067386]
“Better screening and earlier detection of CKD enables earlier use of organ-protective drugs, which may delay progression to end-stage kidney disease [ESKD], thus averting its significant health and economic impacts,” he suggested. [Kidney360 2021;2:1042-1047; Lancet 2020;395:709-733]
Organ-protective treatments underused
Among patients with CKD, use of organ-protective treatments remains
suboptimal. [Lancet 2020;395:709-733; JAMA Netw Open 2019;2:e1918169;
Diabet Med 2016;33:1230-1239]
“In South Korea, for example, SGLT2 inhibitors were used in only 32.9 percent of eligible DKD patients in real-world clinical practice in 2019–2020,” pointed out Yeo. [BMC Nephrol 2021;22:177]
“In the UK, <10 percent of patients with DKD were on SGLT2 inhibitors in 2020,” said Jardine. [Diabetes Care 2022;45:2316-2325]
Cardiorenal benefit of SGLT2 inhibitors in CKD
SGLT2 inhibitors have demonstrated consistent cardiorenal benefits in randomized
controlled trials (RCTs) in CKD patients with or without diabetes mellitus
(DM). [N Engl J Med 2019;380:2295-2306; N Engl J Med 2020;383:1436-1446;
N Engl J Med 2023;388:117-127]
“Among these RCTs, the most recent EMPA-KIDNEY trial of empagliflozin vs placebo had the broadest inclusion criteria, expanding eGFR eligibility to ≥20 mL/min/1.73 m2 and allowing recruitment of patients with normal to moderately increased albuminuria. At baseline, 34.5 percent of patients had eGFR <30 mL/min/1.73 m2, 48.3 percent had urinary albumin-to-creatinine ratio <30 mg/g [A1 category] or ≥30–≤300 mg/g [A2 category], and 54.0 percent had no DM,” said Jardine. [N Engl J Med 2023;388:117-127]
Results showed a 28 percent relative risk reduction (RRR) with empagliflozin vs placebo in the composite primary outcome of kidney disease progression (ie, ESKD, sustained decrease in eGFR to <10 mL/min/1.73 m2, sustained decrease in eGFR of ≥40 percent from baseline, or death from renal causes) or cardiovascular (CV) death (hazard ratio [HR], 0.72; 95 percent confidence interval [CI], 0.64–0.82; p<0.001) after a median follow-up of 2.0 years.
Benefit across eGFR categories, regardless of DM status
In EMPA-KIDNEY, empagliflozin demonstrated consistent cardiorenal
benefit across eGFR categories, regardless of presence or absence of
DM at baseline. (Figure) [N Engl J Med 2023;388:117-127]
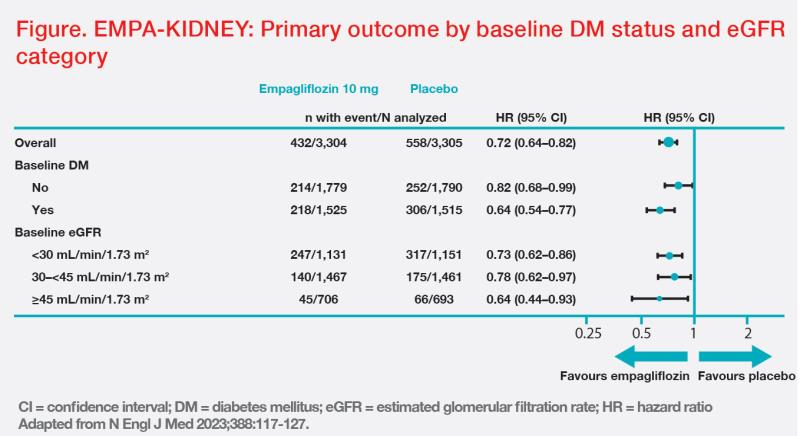
“Until recently, SGLT2 inhibitors were thought not to work in patients with low eGFR, but these results from EMPAKIDNEY and data from another SGLT2 inhibitor trial in CKD indicate greater benefit of SGLT2 inhibitors in higher-risk patients,” said Jardine. [N Engl J Med 2023;388:117-127; J Am Soc Nephrol 2020;31:1128-1139; Clin J Am Soc Nephrol 2021;16:384-395]
“However, given the substantial healthcare burden associated with later stages of CKD, it is important to stop progression of the disease from stage 3,” she added.
If a “typical” 63-year-old CKD patient with eGFR of 56 mL/min/1.73 m2 is started on an SGLT2 inhibitor plus a reninangiotensin-aldosterone system (RAAS) inhibitor, it may be possible to delay ESKD by 15 years vs treatment with a RAAS inhibitor alone, according to extrapolation of long-term benefit based on data from a CKD RCT. [Kidney360 2021:2:1042-1047] “It means that many of these patients may not need dialysis in their lifetime,” suggested Yeo.
DKD guidelines: SGLT2 inhibitors as 1L therapy
2022 guidelines of Kidney Disease: Improving Global Outcomes (KDIGO) recommend
SGLT2 inhibitors as 1L therapy in DKD. [Kidney Int 2022;102:S1-S127]“According to KDIGO, SGLT2 inhibitors
can be used if eGFR is ≥20 mL/min/1.73 m2, and should be continued until
initiation of dialysis,” said Jardine. [Kidney Int 2020;98:S1-S115]
Similarly, based on primary evidence of reducing CKD progression, 2023 guidelines of the American Diabetes Association recommend SGLT2 inhibitors as a preferred 1L treatment in patients with DKD with eGFR ≥20 mL/min/1.73 m2. Once initiated, SGLT2 inhibitor therapy should be continued until dialysis or kidney transplantation. [Diabetes Care 2023;46:S140-S157]
Practical tips on SGLT2 inhibitor use
“Empagliflozin was associated with a lower risk of serious adverse events vs
placebo [HR, 0.92; 95 percent CI, 0.85– 0.99] in EMPA-KIDNEY,” said Jardine. [N Engl J Med 2023;388:117-127]
In RCTs across different patient populations, the small dip in eGFR observed in the first few weeks of SGLT2 inhibitor treatment was followed by stabilization over the next few months. Rates of eGFR decline were slower with SGLT2 inhibitors vs placebo in these trials. [N Engl J Med 2023;388:117-127; N Engl J Med 2020;383:1436-1446; N Engl J Med 2016;375:323-334; J Am Soc Nephrol 2020;31:1128-1139]
“This initial dip in eGFR represents haemodynamic change rather than acute kidney injury [AKI],” pointed out Jardine.“In fact, a meta-analysis of 13 large RCTs of SGLT2 inhibitors [n=90,413; with DM, 82.7 percent] showed that these agents were associated with a 23 percent RRR in AKI [relative risk (RR), 0.77; 95 percent CI, 0.70–0.84].” [Lancet 2022;400:1788-1801]
“This modest initial dip in eGFR is therefore generally not an indication to discontinue SGLT2 inhibitor therapy,” emphasized Yeo. “However, vigilance is needed when combining medications with renal effects that may increase the risk of AKI.”
“As empagliflozin is associated with lower rates of hyperkalaemia vs placebo in DKD patients, particularly those with low eGFR, it may be a good candidate for combined use with drugs that may induce hyperkalaemia,” suggested Jardine. [Diabetes Care 2022;45:1445-1452]
“Patient education is important before starting SGLT2 inhibitor treatment. A recently published Asian-Pacific expert consensus statement provides a useful patient guide on blood pressure control and monitoring, prevention of genitourinary infections, avoidance of ketogenic or very-low-carbohydrate diets, maintenance of adequate hydration, and sick day management,” added Yeo. [Nephrology (Carlton) 2023;28:415-424]
Related MIMS Drugs





 Change Password
Change Password
 Points
Points
 Sign Out
Sign Out


